It’s intern year and you’re on nights in the MICU. You’re always a little bit out of your element when not in the ED. Tonight you get sign out on an older lady with afib and CHF presenting for AMS, being followed by neuro and on BiPAP and critically ill in the CCU; they just gave her a dose of digoxin. Now you ask, “why are they on digoxin?” Because per the fellow “She does really great on digoxin.” You asked because digoxin can make people altered and because you remember that in CHF, digoxin improves symptoms, quality of life, and exercise tolerance and reduces rates of hospitalization and length of stay, but it does not provide a mortality benefit.[1,2] There is also good evidence that patients taking digoxin for atrial fibrillation (afib) have increasing risk of mortality with increasing serum concentrations, even when in the therapeutic range.[2,3] You initially put that aside, since you’re the night intern and have never met the patient, and many more senior doctors have already evaluated the patient and come up with the current plan. It may not be advisable to change plans overnight. About four hours later while rounding, you notice that the patient’s monitor is alarming. You look in from the doorway, and it isn’t clear what is causing the alarm. The nurse then says to you, “Oh, I was signed out that she has frequent PVCs.” Now, you have already decided what to do next. You order a serum digoxin concentration.
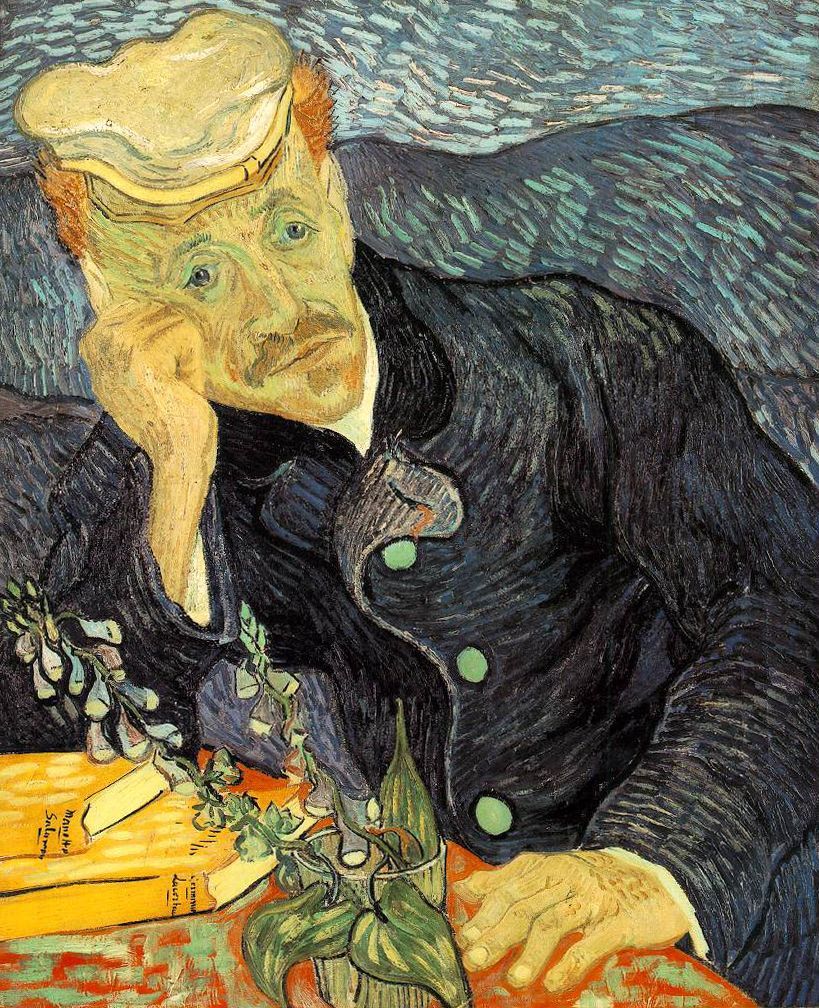
Digoxin Background Digoxin is a cardioactive steroid (CAS). CASs are not only produced by the pharmaceutical industry but are also found in nature in many plants and flowers, including yellow oleander, oleander, dogbane, foxglove, lily of the valley, and red squil. Bufo toads produce a resin that also contains CASs, which some believe to be an aphrodisiac.[4] Image 1: Bufo Toad, Karamell, Common Toad (Bufo bufo), CC BY 3.0 age 2: Yellow Oleander, J.M.Garg, Yellow Oleander (Thevetia peruviana) leaves & flowers in Kolkata W IMG 8008, CC BY-SA 3.0 In 1785, William Withering wrote about digoxin’s effects on the heart.[4] Digoxin is used for atrial tachydysrhythmias and CHF.[4] It has two main modes of action. First, it increases vagal tone, which can be used for ventricular rate control in afib but also can lead to bradycardia, AV block, and bradydysrhythmias. Second, It also inhibits the Na-Ka ATPase pump, which indirectly leads to increased intracellular calcium and increased contractility in CHF. Increased intracellular calcium may also lead to myocardial “irritability” which manifests as ectopy and tachydysrhythmias.[4] Digoxin has a very narrow therapeutic index, about 0.8-2.0 ng/ml historically, and now about 0.5-0.9 ng/ml due to evidence of better outcomes at lower concentrations.[5] It is eliminated mostly by the kidneys, so a small change in GFR can result in supratherapeutic levels despite stable dosing.[4] Patients with digoxin toxicity can present either with acute overdose (the patient takes a handful of pills) or chronic overdose (the patient develops a supratherapeutic concentration while taking a stable dose over time), and these two may differ clinically. In the acute setting, nausea and vomiting are almost always present, while chronically toxic patients develop anorexia as well.[4,6,7] Patients with acute overdose develop lethargy, confusion, and weakness, whereas patients with chronic overdose develop headaches, delirium, confusion, drowsiness, disorientation, visual changes (blurred, halos, and color aberrations towards yellow/green). Though not likely true, some people have theorized that Van Gogh was actually digoxin toxic.[8] Image 3: Van Gogh, Vincent van Gogh, Portrait of Dr. Gachet, marked as public domain, more details on Wikimedia Commons In acute overdose, hyperkalemia is common. Before digoxin-specific FAB – the antidote for CAS toxicity – was available, the rule of 5s was developed: [K] < 5 mmol/L, 100% survive, 5 mmol/L < [K ] < 5.5 mmol/L, 50% survive, and [K ] > 5.5 mmol/L, 100% die.[4] In chronic overdose, hypokalemia is common and increases susceptibility to cardiac toxicity manifested as dysrhythmias.[4] Vagal tone leads to bradydysrhythmias, while myocardial irritability can lead to VF or VT, as well supraventricular tachycardias, including afib and paroxysmal atrial tachycardia with slow ventricular response. Any dysrhythmia other than rapidly conducted atrial tachycardia may occur. Think digoxin when there is increased automaticity with high degree AV block and slow ventricular response, often augmented with PVCs.[6,7] When most people think of ECGs and digoxin, they think of the scooped ST segment or Salvador Dali’s mustache.[7] Image 3: Salvadore Dali, Roger Higgins, World Telegram staff photographer, Salvador Dali NYWTS, marked as public domain, more details on Wikimedia Commons ECG: 1 The Dig Effect https://lifeinthefastlane.com/ecg-library/digoxin-effect/ ECG2: Bidirectional VT https://lifeinthefastlane.com/ecg-library/basics/bvt/ However, the scooped ST segments only are evidence of digoxin presence and not toxicity.[9] The most common ECG finding is actually PVCs, making rhythms like bigeminy and trigeminy common.[7] Bidirectional VT, where you see a beat to beat alternation in the QRS axis (seen below), is pathognomonic for digoxin toxicity.[10] ECG: Bidirectional VT https://lifeinthefastlane.com/ecg-library/basics/bvt/ Digoxin Toxicity Major Risk Factors: Eubacterium latum in the GI tract normally breaks down digoxin, and antibiotics against this bacteria can lead to elevated digoxin concentrations.[11] It is pretty easy for a stable patient on digoxin to easily become an unstable patient on digoxin, especially in an ICU setting, where patients have very high rates of AKI and comorbid conditions.[4,12] What Not to Do and What to Do First, what not to do. Don’t treat hyperkalemia with calcium, because in an animal model of digoxin toxicity, calcium causes “stone heart” – tetanic contraction of the myocardium.4 However, fears of stone heart may be rooted in the way the animal studies were performed, and one recent retrospective study[13] did not show increased mortality with calcium administration. Treating digoxin toxicity with digoxin-specific FAB will also treat the hyperkalemia in that situation. Don’t place a transvenous pacer in a patient with digoxin toxicity, because it can precipitate dysrhythmias in an irritable myocardium.[14,15] Don’t perform gastric lavage, because this increases vagal tone. Don’t replete magnesium in the setting of bradycardia/AV Block, preexisting hypermagnesemia, and renal insufficiency or failure. Now, what to do. Get an ECG and a serum digoxin concentration. If you’re dealing with a CAS other than digoxin, you should see a detectable digoxin concentration, but you won’t be able to use it in a quantitative way. Be sure to check serum electrolytes, including magnesium, and creatinine. Digoxin-specific FAB is the only true definitive treatment. Activated charcoal reduced mortality from yellow oleander poisoning in one study,[16] but this was not reproduced in another.[17,18] Administer atropine for bradycardia to counteract the increased vagal tone. Correct hypokalemia in chronic overdose and magnesium only in the setting of tachydysrhythmias. When to Use digoxin-specific FAB? Whenever there are: How to Treat Digoxin Toxicity Your patient is unstable. She has decreasing alertness after receiving a total of two doses of digoxin over the day and is hypotensive. It isn’t clear whether or not the patient had also been on digoxin as an outpatient. The ECG didn’t show a scooped ST segment, but it did show bigeminy. The digoxin concentration of the patient returns at 3.34 ng/ml about 6 hours after administration of the last dose – well above the therapeutic range but below the hard indications for administration of digoxin-specific FAB. (Concentrations should ideally be measured 6 hours after administration to allow for distribution of the drug.[4] So, now what do you do? Although digoxin-specific FAB is expensive – almost $4000 per vial[19] – in this patient with altered mental status and a likely digoxin-related dysrhythmia, you opt for treating. So, how do you dose digoxin-specific FAB? Each vial binds about 0.5 mg of digoxin. When you have a serum digoxin concentration, you calculate the digoxin-specific FAB dose by multiplying the serum concentration by the weight in kilograms, dividing by 100, and then rounding up to get the number of vials. For the patient in this case: (concentration 3.34 ng/ml) x (weight 109 kg) / 100 = 3.64, which rounds up to 4 vials. If you don’t have a serum concentration, but you know how much was ingested, you can take the amount ingested (mg) divided by 0.5 (mg/bound by a vial). If you can’t get a concentration (or the patient is too unstable to wait for one) you can empirically treat the adult or pediatric patient with 10-20 vials for an acute ingestion, 5 vials for a chronic Adult ingestion, and 2 for a chronic ingestion in a child.[4] One pharmacokinetic study[20] recommends for cardiac arrest giving a full empiric acute toxicity dose or a full calculated dose if a level is available. For an acute overdose without cardiac arrest, they recommend giving 1-2 vials as an initial bolus with additional vials titrated to effect; for chronic overdose, one vial with additional vials to titrate to effect. The authors argue that this dosing regime would likely use less total vials based on pharmacokinetic studies demonstrating 1) a single dose can rapidly eliminate digoxin from the central compartment due to the slow distribution time (>6 hours) and 2) the volume of distribution is variable.[20] This implies that a serum concentration does not accurately predict total body digoxin burden, meaning that current level based dosing over utilizes an expensive antidote.[20] For other CAS, you can’t depend on the serum concentration (though any positive level confirms ingestion), and the digoxin-specific FAB won’t bind with the same affinity. You will likely require more vials. And remember, there is no utility in repeating digoxin levels. You should also monitor patients with severe kidney disease because delayed, recurrent toxicity can occur if the FAB releases the CAS prior to excretion. About one hour after your patient received dig-specific FAB, your nurse barges into the call room and tells you that the patient is doing much better and is now talking. I guess you helped the patient. Important points to remember: References Faculty Reviewer: Sage Wiener, MD





[1] Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med [Internet] 1997;336(8):525–33. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9036306
[2] Vamos M, Erath JW, Hohnloser SH. Digoxin-associated mortality: a systematic review and meta-analysis of the literature. Eur Heart J [Internet] 2015;36(28):1831–8. Available from: https://academic.oup.com/eurheartj/article-lookup/doi/10.1093/eurheartj/ehv143
[3] Lopes RD, Rordorf R, De Ferrari GM, et al. Digoxin and Mortality in Patients With Atrial Fibrillation. J Am Coll Cardiol [Internet] 2018;71(10):1063–74. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29519345
[4] Flomenbaum NE, Goldfrank LR, Hoffman RS, Howland MA, Lewin NA, Nelson LS. Goldfrank’s Toxicologic Emergencies. 8th ed. New York: McGraw-Hill; 2006.
[5] Pincus M. Management of digoxin toxicity. Aust Prescr [Internet] 2016;39(1):18–20. Available from: https://www.nps.org.au/australian-prescriber/articles/management-of-digoxin-toxicity
[6] Nickson C. Digoxin Toxicity [Internet]. Life Fast Lane. 2014;Available from: https://lifeinthefastlane.com/ccc/digoxin-toxicity/
[7] Burns E. Digoxin Toxicity [Internet]. Life Fast Lane ECG Libr. 2017;Available from: https://lifeinthefastlane.com/ecg-library/basics/digoxin-toxicity/
[8] Gruener A. Vincent van Gogh’s yellow vision. Br J Gen Pract [Internet] 2013;63(612):370–1. Available from: http://bjgp.org/cgi/doi/10.3399/bjgp13X669266
[9] Smith SW. ST segment depression: what is the etiology? [Internet]. Dr. Smith’s ECG Blog. 2011;Available from: https://hqmeded-ecg.blogspot.com/2011/04/st-segment-depression-what-is-etiology.html
[10] Burns E. Bidirectional Ventricular Tachycardia [Internet]. Life Fast Lane ECG Libr. 2017;Available from: https://lifeinthefastlane.com/ecg-library/basics/bvt/
[11] Dobkin JF, Saha JR, Butler VP, Neu HC, Lindenbaum J. Inactivation of digoxin by Eubacterium lentum, an anaerobe of the human gut flora. Trans Assoc Am Physicians [Internet] 1982;95:22–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/7182977
[12] Koeze J, Keus F, Dieperink W, van der Horst ICC, Zijlstra JG, van Meurs M. Incidence, timing and outcome of AKI in critically ill patients varies with the definition used and the addition of urine output criteria. BMC Nephrol [Internet] 2017;18(1):70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28219327
[13] Levine M, Nikkanen H, Pallin DJ. The effects of intravenous calcium in patients with digoxin toxicity. J Emerg Med [Internet] 2011;40(1):41–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19201134
[14] Taboulet P, Baud FJ, Bismuth C, Vicaut E. Acute digitalis intoxication–is pacing still appropriate? J Toxicol Clin Toxicol [Internet] 1993;31(2):261–73. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8492339
[15] Taboulet P, Baud FJ, Bismuth C. Clinical features and management of digitalis poisoning–rationale for immunotherapy. J Toxicol Clin Toxicol [Internet] 1993;31(2):247–60. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8492338
[16] Eddleston M, Juszczak E, Buckley NA, et al. Multiple-dose activated charcoal in acute self-poisoning: a randomised controlled trial. Lancet (London, England) [Internet] 2008;371(9612):579–87. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18280328
[17] de Silva HA, Fonseka MMD, Pathmeswaran A, et al. Multiple-dose activated charcoal for treatment of yellow oleander poisoning: a single-blind, randomised, placebo-controlled trial. Lancet (London, England) [Internet] 2003;361(9373):1935–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12801736
[18] Lalonde RL, Deshpande R, Hamilton PP, McLean WM, Greenway DC. Acceleration of digoxin clearance by activated charcoal. Clin Pharmacol Ther [Internet] 1985;37(4):367–71. Available from: http://www.ncbi.nlm.nih.gov/pubmed/3978996
[19] https://www.drugs.com/price-guide/digifab [Internet]. Drugs.com. Available from: https://www.drugs.com/price-guide/digifab
[20] Chan BSH, Buckley NA. Digoxin-specific antibody fragments in the treatment of digoxin toxicity. Clin Toxicol [Internet] 2014;52(8):824–36. Available from: http://www.tandfonline.com/doi/full/10.3109/15563650.2014.943907
Noah Berland
Latest posts by Noah Berland (see all)



1 Comment
ablumenberg · May 1, 2018 at 6:24 pm
Great post!!