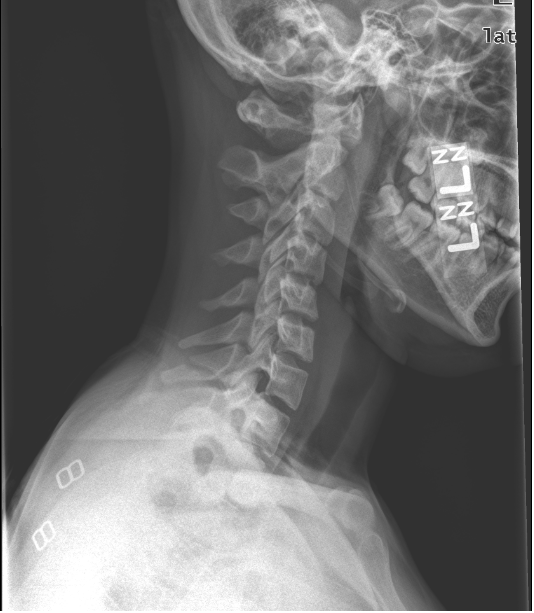
Here was our original image:
Before we get to the full interpretation here is some background. The patient actually presented to another emergency department after a car accident. They were the back seat passenger on the non-driver’s side and the car was hit on the driver’s side by an ambulance. They were noted to have syncope after the accident. Part of the mechanism was that the patient’s head hit the car ceiling. They were evaluated in the ED and sent home. The patient complained of persistent pain and presented to the King’s County ED 3 days later.
Briefly, the basics to reading C-spine films are as follows:
- Is it an adequate film – First look for good visualization of all 7 cervical vertebra and the C7-T1 interface. Next, look for good alignment of the lateral masses to evaluate for rotation
- Check for alignment of the anterior and posterior longitudinal ligaments, spinolaminar lines and spinous process line
- Atlantodens interval (<3mm for adults <5mm in children)
- Retropharyngeal space (C1-2) = 7-8mm
- Pretracheal space (C6) – 22mm adult, 14mm child

If you stopped there, then you made the common cognitive error of satisfaction of search. But look a little closer at the pre-vertebral space and you will see that it is significantly larger than normal. With a width of 11mm at C2 that’s significantly more than the normal of 7-8mml. The AP and open mouth views for this patient are both inadequate films with significant rotation. This along with the fact that there is significant prevertebral swelling at C2 but not at C6 suggests an additional injury in the upper cervical spine and prompts further imaging and C-spine immobilization.
In this patient, the CT scan showed the following:
Video of CT here
Now we can clearly see that the cause of the increased prevertebral swelling at C1-2 is a Jefferson Fracture! This patient also has a type II odontoid fracture.
A Jefferson fracture (AKA burst fracture of the ring of C1) is usually caused by an axial loading transferred through the occipital condyles to the superior articular surfaces of the lateral masses of C1. As in any ring, you will typically see fractures in multiple locations since it is difficult to break a ring in only one location. Excess pressure on the lateral masses of C1 will result in fracture of the anterior and posterior arches.
Radiographcially, on the odontoid view, this will manifest as lateral displacement of the lateral masses, increasing the space between the dens and the lateral mass. The normal space is 2mm but displacement of more than 7mm is associated with complete disruption of the transverse ligament.
The type II odontoid fracture adds another level of complexity to this patient’s management. Usually caused by a hyperflexion or hyperextension injury, this particular type of dens fracture can lead to a compromised blood flow to the dens. Patients may have high cervical pain with muscle spasm and neurologic symptoms (18-25% of patients) ranging from sensory loss to quadriplegia. The classification of odontoid fractures is seen below:
An important distinction to make is the difference between type 2 and type 3 fractures. One specific area to evaluate on the lateral C-spine film is the “ring of C2” which is formed by the superior articular facet and the transverse process of C2 projecting laterally. Seen below, if the dens fracture causes a disruption of this ring, then it is likely a type 3 fracture.
The management of this injury obviously requires prompt neurosurgical consultation after dealing with the ABC’s for this trauma patient. Definitive management depends on the degree of stability of the fracture. When considering the Jefferson fracture alone, stability is defined by whether the transverse ligament is intact. An intact ligament can be managed by the use of a cervical collar (hard or soft) worn during the healing process. However, a disrupted ligament requires traction with the use of a rigid halo or surgery (Fusion of C1-C3). The type 2 dens fracture is also considered unstable and requires halo immobilization. Risk factors for non-union include significant displacement of the dens (>5mm), posterior displacement, age > 65 and comminution.
When the type 2 dens fracture occurs with the Jefferson fracture, a halovest can be used for initial management and if the dens fracture does not heal a C1-C2 fusion can be performed. However, if the transverse ligament is ruptured the halovest alone is not sufficient since the transverse ligament is not there to hold the dens in place to allow for healing. In this case, operative management with C1-C3 fusion is the best option.
Our patient was admitted to the SICU for neurologic monitoring and underwent halovest placement. Although she had a type 2 dens fracture and Jefferson fracture, the dens was not significantly displaced and the transverse ligament was intact. She responded well to treatment and her repeat Cspine CT ~5 months later is shown below:
References:
Wheeless’ Textbook of Orthopaedics online
Tintinalli’s Emergency Medicine: A Comprehensive Study Guide
http://nypemergency.org/reading_emergency_images/c-spine.html
Medscape: Cervical Spine Fracture in Emergency Medicine
nchristopher
Latest posts by nchristopher (see all)
- What’s wrong with this picture? – Answer - September 11, 2013
- What’s wrong with this picture? - August 21, 2013
- EKG Case 8 – Answer - July 16, 2013












1 Comment
Carl · July 26, 2012 at 12:46 pm
Great case, I can never remember these fractures.