
A 20 year-old man with no PMH presents to the ED after skateboarding injury. He states he was skateboarding around a construction site when he felt a sharp object cut the back of his right leg. Vitals are within normal limits.
What do you see?What structures are you concerned about?
Achilles tendon injury/ rupture
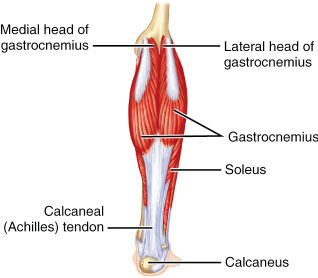
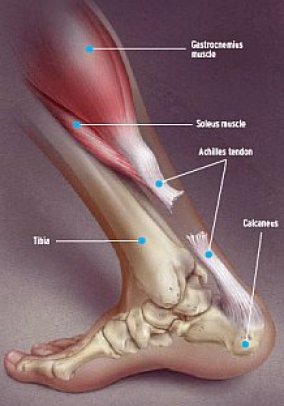
- Anatomy: The Achilles tendon (calcaneal tendon) attaches several muscles from the posterior leg to the calcaneus. These muscles include gastrocnemius, soleus, and plantaris. When these muscles are activated, it causes the foot to plantar flex at the ankle.
- Achilles tendon rupture mechanisms:
- Penetrating trauma like in this patient
- Usually occurs from blunt or sports-related trauma – think the “episodic athlete”, a person who normally does not exercise and attempts to engage in physical activity.
- Forced plantar flexion
- Sudden dorsiflexion in a plantar flexed foot
- Usually accompanied with a “pop” sensation
What physical exam finding may help you?
Thompson Test
Have the patient in prone position with foot hanging off the stretcher and then squeeze the calf. Normally, you should see plantar flexion of the foot if the Achilles tendon is intact. This motion may be absent if there is complete rupture of the tendon.
What would be your workup in the ED?
- Always go through your ABCDEs.
- Labs: Pre-operative tests for surgery
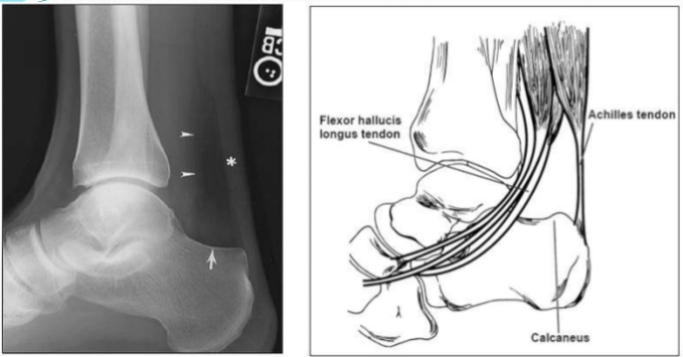
- Imaging: In this case, since the patient has an open wound, it would be a good idea to get an x-ray to make sure there aren’t any foreign bodies
- Triangle of Kager: Radiographic triangle formed by the Achilles, calcaneus, and tibia. Injury to the Achilles (or ankle in general) can cause blood to pool in this area creating a dark triangle on imaging.
What will you do for our patient in the ED? What is the definitive treatment?
- Pain control!
- Don’t forget Tdap vaccination!
- Antibiotic prophylaxis may be a good idea for a wound this size, especially since construction sites are not the most sterile of environments. 1-2 grams of cefazolin is often given, but pressure irrigation with saline will be most important in infection prevention.
- Surgery vs. Non-operative care: In cases of closed achilles tendon rupture, there is debate about operative vs non-operative treatment. Surgical repairs result in more rapid healing time and lower rates of recurrent rupture. Advocates of conservative treatment state that there is no long-term difference in power, range of motion, and function with nonsurgical treatment, and patients do not incur risk of possible surgical complications such as infection. Patients who are not admitted for immediate surgery should be splinted in equinus (plantar flexed) and follow-up with orthopedics.
- Back to our patient: He will likely have surgical repair since his wound is already open, and contamination may be asssumed. He likely needs a wash out of the area regardless.
What is our disposition for this patient?
Admit for immediate surgery vs washout, laceration repair, plantar flex splint, and orthopedic follow-up.
References:
Karadshes,M. Achilles Tendon Rupture. Othrobullets. http://www.orthobullets.com/foot-and-ankle/7021/achilles-tendon-rupture
Mittal,A. Management of TendoAchilles Rupture. http://www.slideshare.net/mittal87/management-of-tendoachillis-rupture
Karen
Latest posts by Karen (see all)
- Don’t Clam Up: Emergent Thoracotomy - March 13, 2017
- Black and Blue and Red All Over: Management of Acute Limb Ischemia - February 7, 2017
- Bored and Toxic: Toxic Shock Syndrome - January 24, 2017



5 Comments
ablumenberg · October 8, 2016 at 12:07 am
With thorough irrigation would prophylactic antibiotics truly be beneficial?
Ian deSouza · October 8, 2016 at 6:46 pm
Good point Blumenberg. Probably not, but this is a “complicated wound” – deep with visible tendon rupture and “what not”. Most studies that demonstrate no benefit of prophylactic antibiosis involve wounds that are “uncomplicated”.
ablumenberg · October 9, 2016 at 10:36 am
Agreed, and I probably would put this patient on prophylactic antibiotics in real life, but there is an argument to be made that prophylactic antibiotics do not decrease the rate of infection and only change the epidemiology of drug resistant infections in complex lacerations.
Aggressive irrigation is known to decrease infection risk and has no substantial adverse effects. Karen emphasized this nicely in the case presentation. That leg needs to go under the faucet!
Ian deSouza · October 9, 2016 at 3:21 pm
Probably true, but to date, there is no evidence to support that logical argument. The specific question of administering antibiotic prophylaxis for “complicated” lacerations has not been studied. That is really the point I was trying to make.
One could (and commonly does) pose a counter-argument that wound is contaminated and needs antibiotics to prevent a deep space infection/abscess and/or failed surgical outcome. It becomes a risk/benefit analysis, somewhat subjective (especially if you are the one who will operate) without any data.
dzeccola · October 9, 2016 at 10:39 pm
Yea, if it was nice clean gash…maybe. But that’s a beefy wood with rough edges. I’m not sure I could be confident I really got that clean enough to not give Abx.