It’s a busy night shift when a nurse alerts you to an elderly patient sent from a nursing home who is hypotensive, tachycardic, tachypneic, febrile, altered, and appears dehydrated. You assume sepsis, send labs, begin treating empirically with broad spectrum antibiotics, and start fluid resuscitating the patient. Despite receiving 30cc/kg of normal saline, she remains altered and hypotensive so you throw in a central line and begin norepinephrine and consult the ICU. Labs show a lactate of 5, WBC of 18k, and the chest x-ray shows a whopping pneumonia. The nurse lets you know that she has been titrating up the drip but the blood pressure is not responding, so you add on vasopressin and sign out the patient to the ICU team. After some time, the patient codes and while you are able get ROSC, the patient continues to be hypotensive despite numerous liters of fluids and maxed out norepinephrine and vasopressin.
As you stand there, glad that you wore your brown pants, the nurse asks, “what do we do next?”

How about trying some…
This literature review was limited to human studies in English.
Mechanism of action
Methylene blue (MB) is a dye that has numerous intracellular actions. When used as a treatment for methemoglobinemia, it is converted by NADPH methemoglobin reductase to leucomethylene blue, which then reduces the iron in heme, restoring its oxygen carrying capacity (1). It inhibits guanylate cyclase, an enzyme that produces cyclic guanosine monophosphate (cGMP), which decreases intracellular calcium concentrations, activates potassium channels, and activates a protein kinase that activates myosin light chain phosphatase, all of which lead to relaxation of smooth muscle. MB also scavenges and inhibits nitric oxide, and these actions within the same pathway lead to increased cGMP levels (2,3). The production of nitric oxide is a common endpoint for multiple etiologies that cause vasodilation. Thus, MB works to inhibit vascular smooth muscle relaxation, particularly in patients with excessive nitric oxide production.
Evidence
Postop VasoplegiaMethylene blue has been in use for postoperative vasoplegia for decades. Evora reviewed the literature for this indication of methylene blue in 2015, concluding that while MB was safe and should be used in select cases of vasoplegia, additional studies were needed to find the optimal timing of dosing (4). This vasoplegic syndrome is unlikely to be encountered in the Emergency Department as it is most often seen in patients that have just undergone cardiothoracic surgery.

A review by Lo, et al in 2014 looked at the available data until 2012 and concluded that methylene blue may be a useful adjunct to vasopressors in shock due to sepsis (n=159), overdose (n=1), or anaphylaxis (n=9) (5). Limitations of this review include the use of numerous case reports with only two RCTs, and significant heterogeneity with regard to patient population, study design, MB dosage, vasopressor use, timing of administration, and clinically oriented outcomes. However, there was a universal improvement in BP or MAP of patients who received MB. These effects on MAP were also confirmed by a systematic review of 5 RCTs that included the two evaluated by Lo and 3 others involving postoperative patients (6). In the studies that examined it, vasopressor requirements were significantly decreased with MB administration. The two RCTs (7,8) did not show a significant mortality difference between treatment groups, but these studies may not have been sufficiently powered to detect such a difference. Pasin et. al also noted there was no significant effect on mortality with MB.
Since these reviews, Abd-Alhameed, et al in 2014 conducted a small RCT (n=40) in which the treatment group received methylene blue via bolus followed by a 4-hour infusion and the control group received normal saline. All patients met severe sepsis or septic shock criteria, and required pressor support. There was a significant difference in the MAP between groups from 2 – 24 hours after infusion (9). Cardiac output and SVR were also significantly higher in the MB group in the same time interval. The MB group also required significantly less pressors, shorter ICU length-of-stay, and significantly lower mortality. This study was unique in that methylene blue was not studied as a rescue medication for refractory shock but rather was initiated once the patient required at least 0.2 ug/kg/min of norepinephrine.
There are case reports of methylene blue being used to successfully treat patients who presented with anaphylaxis from various agents, such as protamine, aprotinin, penicillin, and radiocontrast. All of these patients had received standard therapy with epinephrine and steroids. In some cases, additional pressors were given without improvement in hypotension or urticaria until MB was started (5). It is worth noting that the reactions to radiocontrast were likely anaphylactoid reactions as true IgE-mediated anaphylaxis to radiocontrast is unlikely. Jang, et. al reported a case of shock due to amlodipine overdose that was refractory to 3L NS, calcium gluconate, glucagon, dopamine, norepinephrine, and high dose insulin drip. Improvement in BP was noted 1 hour into MB infusion, allowing weaning of insulin and vasopressors (3).
Adverse Effects
MiscMB has long been used as a treatment for methemoglobinemia, but it can paradoxically cause methemoglobinemia when used in excess (1,10). Juffermans, et al. performed a small study (n=15) to evaluate for the effects of MB at different dosages and found that higher doses (7+ mg/kg) may compromise splanchnic perfusion (11). In patients with G6PD deficiency, MB can induce hemolytic anemia (1). It is also known to cause a temporary blue-greenish discoloration of skin and secretions and should be used cautiously in patients with severe renal impairment (12).

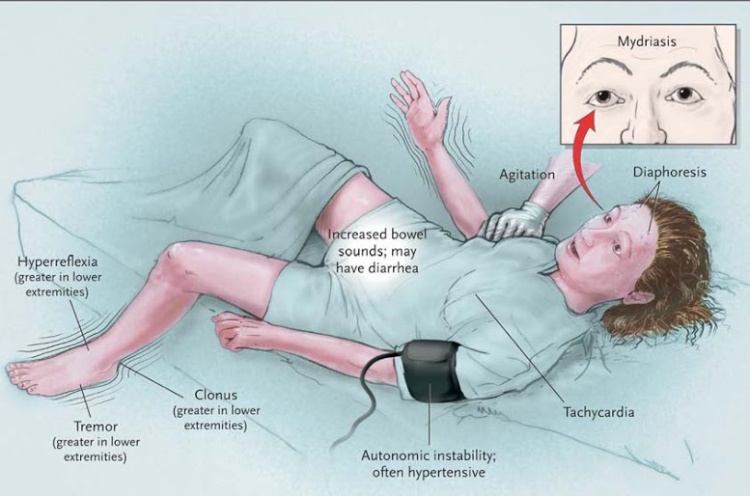
A number of case reports have identified a range of symptoms including vomiting, aphasia, confusion, and agitation that develop in post-op parathyroidectomy patients who had received MB for parathyroid staining. The association between methylene blue and psychotropic medications, especially those that affect serotonin levels, was discovered as the number of these cases grew (13). The FDA has since put out a safety communication on the potential interaction between MB and serotonergic medications. These patients developed a syndrome similar to serotonin syndrome that generally resolved within 48-96 hours. Not all patients on SSRIs who received MB developed this syndrome, however, suggesting that there may be another factor at play (14). A similar presentation with outright serotonin syndrome was also seen in patients receiving MB for vasoplegia status post cardiac surgery (15).
Weiner, et. al performed a single-center, retrospective review of postop patients that received MB with propensity score matching, which concluded that MB is independently associated with poor outcomes (16). However, this study had multiple methodological problems limiting its validity and the reported increased mortality was not replicated in propensity matching.
Conclusion

Patients with refractory hypotension have poor outcomes. MB is a cheap tool in our armamentarium for properly selected patients. The evidence supporting the use of methylene blue seems to indicate that it improves hemodynamic parameters, but its effect on mortality is questionable. It is contraindicated in patients with G6PD deficiency and patients taking any medications that may increase serum serotonin levels. There is marked variation in dosing regimens in the literature, but a safe starting point would be similar to the ones used for methemoglobinemia or vasoplegic syndrome (1-2 mg/kg over 5-60 minutes with slower infusions used for vasoplegia). This would avoid the dose-dependent adverse effects discussed above.
Methylene blue should be considered in refractory hypotension of any etiology, but the strongest evidence exists for septic shock and post-op vasoplegia. The evidence is scant but it may be helpful in anaphylaxis/anaphylactoid reactions or toxic ingestions of beta blockers or calcium channel blockers. Keep in mind, none of these studies evaluated MB in cardiogenic or hypovolemic shock. Larger scale studies need to be performed in order to determine if there is a mortality benefit of increasing MAP with MB. Further studies should also look at optimal dosing regimens and timing of administration.
TL;DR

Peer Reviewers: Wendy Chan, MD and Raul Hernandez, MD
Faculty Advisor: Ian deSouza, MD
References
- Sikka P, Bindra V, Kapoor S, Jain V, Saxena K. Blue cures blue but be cautious. Journal Of Pharmacy & Bioallied Sciences [serial online]. October 2011;3(4):543-545.
- Francis SH, Busch JL, Corbin JD. cGMP-Dependent Protein Kinases and cGMP Phosphodiesterases in Nitric Oxide and cGMP Action. Sibley D, ed. Pharmacological Reviews. 2010;62(3):525-563.
- Jang D, Nelson L, Hoffman R. Methylene blue in the treatment of refractory shock from an amlodipine overdose. Annals Of Emergency Medicine [serial online]. December 2011;58(6):565-567.
- Evora PRB, Alves L, Ferreira CA, et al. Twenty years of vasoplegic syndrome treatment in heart surgery. Methylene blue revised. Revista Brasileira de Cirurgia Cardiovascular : órgão oficial da Sociedade Brasileira de Cirurgia Cardiovascular. 2015;30(1):84-92. doi:10.5935/1678-9741.20140115.
- Lo J, Darracq M, Clark R. Pharmacology in Emergency Medicine: A Review of Methylene Blue Treatment for Cardiovascular Collapse. Journal Of Emergency Medicine [serial online]. May 1, 2014;46:670-679.
- Pasin L, Umbrello M, Landoni G, et al. Methylene blue as a vasopressor: a meta-analysis of randomised trials. Critical Care And Resuscitation: Journal Of The Australasian Academy Of Critical Care Medicine [serial online]. March 2013;15(1):42-48.
- Kirov MY, Evgenov OV, Evgenov NV, et al. Infusion of methylene blue in human septic shock: a pilot, randomized, controlled study. Crit Care Med 2001;29:1860–7.
- Memis D, Karamanlioglu B, Yuksel M, Gemlik I, Pamukcu Z. The influence of methylene blue infusion on cytokine levels during severe sepsis. Anaesth Intensive Care 2002;30:755–62.
- Abd-Alhameed AE, Hamed AM, Omran AS. Methylene blue: Role in early management of septic shock patients?. Ain-Shams J Anaesthesiol 2014;7:327-35.
- Consider methylene blue when treating acquired methaemoglobinaemia. Drugs & Therapy Perspectives [serial online]. May 2014;30(5):185-188.
- Juffermans N, Vervloet M, Daemen-Gubbels C, Binnekade J, Jong M, Groeneveld A. A dose-finding study of methylene blue to inhibit nitric oxide actions in the hemodynamics of human septic shock. Nitric Oxide [serial online]. January 1, 2010;22:275-280.
- Methylene Blue. Lexicomp. Retrieved from: http://online.lexi.com/lco/action/doc/retrieve/docid/patch_f/7279.
- Ng B, Cameron A. Review Article: The Role of Methylene Blue in Serotonin Syndrome: A Systematic Review. Psychosomatics [serial online]. January 1, 2010;51:194-200.
- Shopes E, Gerard W, Baughman J. Methylene Blue Encephalopathy: A Case Report and Review of Published Cases. AANA Journal [serial online]. June 2013;81(3):215-221
- Martino E, Winterton D, Landoni G, et al. Original Article: The Blue Coma: The Role of Methylene Blue in Unexplained Coma After Cardiac Surgery: A Case Series. Journal Of Cardiothoracic And Vascular Anesthesia [serial online]. January 1, 2015.
- Weiner M, Lin H, Danforth D, Rao S, Hosseinian L, Fischer G. ORIGINAL ARTICLE: Methylene Blue is Associated With Poor Outcomes in Vasoplegic Shock. Journal Of Cardiothoracic And Vascular Anesthesia [serial online]. December 1, 2013;27:1233-1238.
edenkim
Latest posts by edenkim (see all)
- Cracking Skulls: When is Neurosurgical Intervention Helpful for ICH? - October 1, 2017
- Valproic Acid Toxicity – The evidence behind different treatment options - July 5, 2017
- Thyroid Storm – How to Recognize It and How to Treat It - June 4, 2017




4 Comments
wendy · March 21, 2016 at 6:32 pm
Great post! I was talking with another resident and we agreed based on your evidence that potentially reversible forms of refractory shock (like anaphylaxis) would be a great time to reach for the metblue. i’m a little more skeptical of pressor resistent septic shock because the prognosis is so bad and ?bump in MAP is unlikely to change the downward spiral.
edenkim · March 22, 2016 at 3:35 am
Thanks! Although I wonder if MB is used earlier on in septic shock like in the Abd-Alheem trial, we might be able to blunt or prevent that downward spiral altogether by avoiding prolonged hypoperfusion. Even if they’re already on the way down, MB may still have a role (as long as it’s safe in that patient) since there’s not much else you can do. At the very least it could decrease the amount of pressors and/or fluids needed to maintain perfusion while antibiotics work on source control.
Kylie Birnbaum · March 21, 2016 at 9:49 pm
Wow, that blue song was stuck in my head for the entirety of 1999. Now it’s back in my head again… Thanks, Eden.
edenkim · March 22, 2016 at 3:36 am
YES! How amazing is that music video?